Tendinitis vs. Tendinosis: What’s the Difference?
If you’ve ever had nagging elbow pain after a long weekend of yard work, or your Achilles tendon screaming at you after ramping up your mileage too quickly, you may have heard the term “tendinitis” tossed around. It’s the go-to explanation for tendon pain—but here’s the plot twist: not all tendon pain is actually tendinitis. Sometimes, it’s tendinosis.
While the names sound almost identical, these conditions are very different. Understanding which one you’re dealing with is key to proper treatment, preventing reinjury, and speeding up recovery. Let’s break it down in a way that makes sense (no medical degree required).
First Things First: What’s a Tendon?
Tendons are the strong, fibrous cords that connect muscle to bone. They act as transmitters, helping muscles generate the force needed for movement. Imagine them like high-strength climbing ropes—flexible, durable, and capable of withstanding a lot of tension.
But even ropes have their limits. Put too much stress on a tendon too quickly, or repeat the same motion over and over without enough rest, and you can end up with microscopic damage. If your body doesn’t get a chance to repair that damage, pain and dysfunction soon follow.
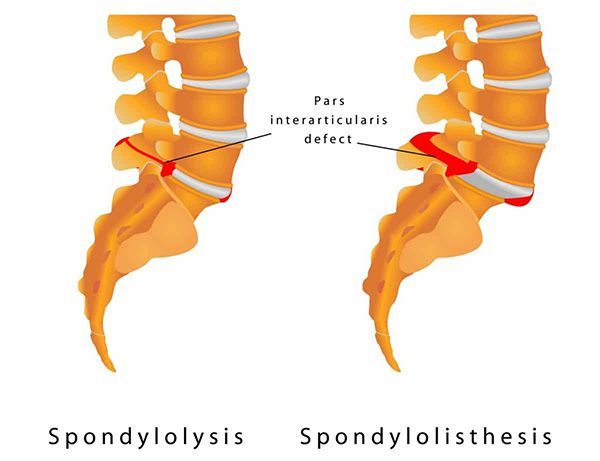
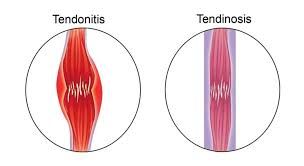
Tendinitis: The “Hot” Injury
The suffix “-itis” means inflammation, and that’s exactly what tendinitis is: inflammation of a tendon. This is the body’s short-term alarm system. When you overdo it—say you spend hours weeding your garden when you’re usually behind a desk—the tendon fibers get irritated, and your body rushes in with an inflammatory response.
Symptoms of Tendinitis:
- Sharp, localized pain during movement
- Swelling or mild puffiness
- Warmth or redness around the tendon
- Pain that’s usually worse with activity, but may ease with rest
Tendinitis is an acute injury, meaning it tends to show up suddenly and intensely. The good news? With the right care, it usually improves within a few weeks.
Treatment for Tendinitis
Because tendinitis is an inflammatory condition, treatment focuses on calming things down:
- Rest and activity modification – Give the tendon a break from the activity that triggered the flare-up.
- Ice – Helps reduce swelling and discomfort.
- Gentle stretching – Keeps the area from stiffening up.
- Massage therapy – Improves blood flow and reduces surrounding muscle tension.
- Chiropractic care – Restores proper joint alignment to minimize mechanical stress on the tendon.
Tendinosis: The “Stubborn” Injury
Now, here’s where things get tricky. If tendon pain lingers for months instead of weeks, you may not be dealing with inflammation anymore. Instead, the tendon itself has started to break down. This is tendinosis.
Tendinosis is a degenerative condition, meaning the tendon fibers are wearing down over time due to repetitive stress and inadequate healing. Unlike tendinitis, there’s no active inflammation—just a tendon that’s become structurally weaker.
Symptoms of Tendinosis:
- A dull, aching pain that builds gradually
- Stiffness, especially in the morning or after rest
- Pain that may persist even after activity stops
- Tenderness when pressing on the tendon
- Thickening or a “lumpy” feel in the tendon
Tendinosis is more frustrating because it doesn’t resolve with just a few weeks of rest. The tendon needs active rehabilitation to encourage new, healthy tissue to replace the damaged fibers.
Treatment for Tendinosis
Because the issue is degeneration rather than inflammation, treatment looks different:
- Eccentric strengthening exercises – Slowly lengthening the muscle under load (think heel drops for Achilles tendinosis) stimulates tendon remodeling.
- Soft tissue therapy – Techniques like massage or instrument-assisted mobilization help increase blood flow.
- Chiropractic adjustments – Improve biomechanics to reduce abnormal stress on the tendon.
- Nutritional support – Collagen and vitamin C can assist tissue healing.
- Gradual loading – A carefully structured return-to-activity program helps build tendon resilience.
Why the Difference Matters
This is where many people go wrong. Tendinitis and tendinosis both cause tendon pain, but they require different management strategies.
- Treating tendinosis like tendinitis(resting, icing, and waiting it out) won’t solve the problem—it may even make it worse by allowing further degeneration.
- Treating tendinitis like tendinosis(jumping into aggressive exercise too soon) can prolong the inflammation and increase pain.
That’s why getting the right diagnosis matters. The right treatment depends on whether your tendon is inflamed (tendinitis) or breaking down (tendinosis).
Common Areas Where Tendon Trouble Strikes
This is paragraph text. Click it or hit the Manage Text button to change the font, color, size, format, and more. To set up site-wide paragraph and title styles, go to Site Theme.
- Elbow – “Tennis elbow” (lateral epicondylitis/tendinosis) and “golfer’s elbow” (medial epicondylitis).
- Shoulder – Rotator cuff tendons are frequent victims of overuse.
- Achilles tendon – Often stressed in runners, jumpers, and anyone upping their activity suddenly.
- Knee – Patellar tendon pain, sometimes called “jumper’s knee.”
- Wrist – Common in desk workers, athletes, and anyone doing repetitive gripping.
Where Chiropractic and Massage Come In
Chiropractic care and massage therapy are powerful partners when it comes to managing tendon injuries. Here’s how:
- Chiropractic care helps by addressing underlying joint and movement dysfunctions. If your ankle doesn’t move properly, your Achilles tendon takes the brunt. If your shoulder mechanics are off, your rotator cuff pays the price. Correcting these issues helps unload the tendon and reduce the risk of reinjury.
- Massage therapy boosts circulation, improves flexibility, and decreases muscle tension around the tendon. This can speed up healing, especially in tendinosis cases where blood flow is often limited.
Together, these approaches not only treat the pain but also target the “why” behind it—so you can get back to your favorite activities with fewer setbacks.
How to Protect Your Tendons
Prevention is always better than rehab. Here are a few tendon-friendly habits:
- Warm up properly before activity to prepare muscles and tendons.
- Increase intensity gradually —avoid sudden spikes in exercise volume.
- Cross-train to prevent overloading the same tendon day after day.
- Strength train —especially eccentric exercises—to keep tendons strong.
- Listen to your body —don’t push through sharp tendon pain.
The Bottom Line
Tendon pain isn’t one-size-fits-all.
- Tendinitis= inflammation (short-term, “hot” injury).
- Tendinosis= degeneration (long-term, “stubborn” injury).
Knowing the difference makes all the difference for recovery. If your tendon pain has hung around longer than a couple of weeks, it may be more than just “tendinitis.”
Don’t play the guessing game. A chiropractor or massage therapist can help determine what’s really going on and create a personalized plan to get you back to moving comfortably.
So whether it’s your elbow, shoulder, knee, or Achilles that’s giving you grief, let us help you untangle tendon trouble—before it ties you in knots.
Bethany Wolcott
D’Youville Chiropractic ‘26