Runner’s Knee: What It Is, Why It Happens, and How to Keep On Running

If you’ve ever gone for a run and come home with an achy, nagging pain around your knee, you might have experienced the all-too-common condition known as Runner’s Knee. But don’t let the name fool you — you don’t have to be a marathoner to be affected. Runner’s Knee can strike casual joggers, weekend warriors, or even people who rarely run but take a long walk or hike.
At Peak Performance, we see lots of patients who are sidelined by this pesky knee pain. The good news? It’s treatable, manageable, and very often preventable. Let’s dive into what Runner’s Knee actually is, how it occurs, how to treat it, and how to keep it from coming back.
What Is Runner’s Knee?
Runner’s Knee is the layperson’s term for patellofemoral pain syndrome (PFPS). In short, it’s pain at the front of the knee, around or behind the kneecap (patella). It typically presents as a dull, aching pain that worsens with activities like running, squatting, going up or down stairs, or even sitting with your knees bent for long periods (think movie theater syndrome!).
You might also experience:
- A grinding or clicking sensation under the kneecap
- Tenderness around the kneecap
- Mild swelling
How Does It Happen?
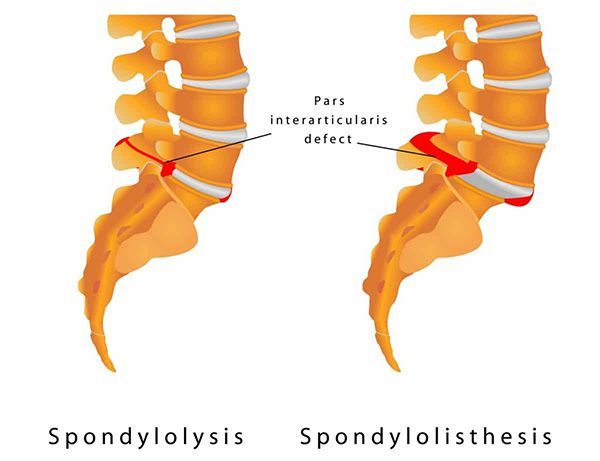
The knee is a complex joint with a lot of moving parts — bones, muscles, tendons, ligaments, and cartilage all need to work in harmony. The patella rides along a groove at the end of your femur (thigh bone). Ideally, it should glide smoothly. But sometimes, due to muscle imbalances, overuse, or poor movement mechanics, the patella is pulled out of its ideal alignment, causing friction and irritation.
Here are some of the most common causes:
Overuse
Logging lots of miles without proper rest can cause repetitive stress on the knee joint. This is why new runners or those increasing mileage too quickly often encounter Runner’s Knee.
Muscle Imbalances
Weakness in the glutes, hips, or quadriceps can throw off the mechanics of your lower body, causing the knee to track poorly. Tight hamstrings and calves can also contribute.
Poor Foot Mechanics
Flat feet, overpronation, or poorly supported footwear can create misalignment from the ground up, putting extra strain on the knees.
Improper Training
Suddenly changing your training routine, running on uneven surfaces, or wearing old, worn-out shoes can all increase the risk.
Structural Factors
Some people simply have anatomical differences — such as wider hips or a shallow patellar groove — that make them more prone to developing Runner’s Knee.
How Do You Treat It?
Here’s the good news: Runner’s Knee is usually very treatable without surgery. In fact, most cases improve with a combination of rest, targeted exercises, manual therapy, and sometimes simple lifestyle changes. Here’s how we typically approach it:
1. Rest and Activity Modification
First things first — if your knee is screaming at you, it’s time to listen. Taking a short break from high-impact activities allows inflammation to calm down. But rest doesn’t mean total inactivity; low-impact exercises like swimming or cycling (if pain-free) can keep you moving.
2. Ice and Elevation
Applying ice for 15-20 minutes a few times a day can help reduce swelling and pain in the early stages.
3. Chiropractic Care
Chiropractic adjustments can improve joint mobility in the hips, pelvis, and lower back, which in turn can help correct faulty knee mechanics. Your chiropractor will also evaluate your gait and posture to identify contributing factors.
4. Massage Therapy
Targeted massage can help release tight muscles, improve blood flow, and promote healing. We often see tightness in the quads, hamstrings, calves, and iliotibial (IT) band in patients with Runner’s Knee — all of which can benefit from skilled hands-on work.
5. Corrective Exercises
Strengthening weak muscles (especially the glutes and hips) and improving flexibility are key to long-term recovery. Here are a few staples we often recommend:
- Glute bridges
- Clamshells
- Side-lying leg lifts
- Foam rolling for the quads, hamstrings, calves, and IT band
- Quadriceps and hamstring stretches
6. Footwear and Orthotics
Wearing proper running shoes with adequate support can make a world of difference. In some cases, custom orthotics can help correct foot mechanics and reduce knee strain.
How Can You Prevent It?
Once your knee is feeling better, the next goal is to keep it that way! Prevention is all about addressing the factors that contributed to the issue in the first place.
1. Strength Training
Incorporate strength training 2-3 times a week to build resilience in your hips, glutes, and core. Strong muscles help control knee movement and absorb impact.
2. Gradual Progression
Follow the “10% rule”: don’t increase your weekly running mileage by more than 10% per week. Sudden jumps in volume are a major trigger for Runner’s Knee.
3. Mix Up Your Workouts
Cross-training (like cycling, swimming, or strength training) helps reduce repetitive stress on your knees while keeping your fitness up.
4. Warm Up and Cool Down
Dynamic warm-ups and mobility exercises prepare your joints and muscles for activity. After your run, take time to stretch and foam roll.
5. Pay Attention to Footwear
Replace running shoes every 300-500 miles, and make sure they fit well and provide the right level of support for your foot type.
6. Listen to Your Body
If you feel early signs of knee discomfort, don’t ignore them. Rest, adjust your training, and seek care before it turns into a bigger issue.
When to See a Pro
If your knee pain persists despite rest and self-care, it’s time to get it checked out. At Peak Performance, our chiropractors and massage therapists work as a team to evaluate your movement patterns, identify imbalances, and provide a personalized treatment plan to get you back on track — and back on the road.
Runner’s Knee doesn’t have to be the end of your running journey. With the right treatment and smart prevention strategies, you can enjoy many more miles pain-free. So lace up those shoes — and if your knees need a little TLC along the way, we’ve got your back (and your knees!).
Bethany Wolcott
D’Youville Chiropractic ‘26